Study Identifies Who Is Most at-Risk For Opioid Abuse
Fact checked by Nick Blackmer

Key Takeaways
- Although the opioid epidemic is nationwide, researchers have identified 25 hot spots throughout the country that are disproportionately affected.
- White males in their late 20s and early 30s are the most affected by opioid use disorder.
- Researchers also found that mental distress increased the risk of dying from a drug overdose by as much as 39%.
Although the opioid epidemic is a problem nationwide, it isn’t affecting the whole country equally. A new study finds that the crisis is disproportionately impacting certain hot spots and is most widespread in six states.1
This latest research, conducted by researchers at the University of Cincinnati, looked at national data on opioid deaths in the United States. They found that although some states have been hit particularly hard by the epidemic, there are 25 smaller hot spots of fatal opioid overdoses within those regions where health organizations should be concentrating their efforts.
By digging deeper into the statistics, the researchers also found that several factors like age, gender, and mental distress can up a person’s risk for abusing opioids. The May study was published in the journal PLOS One.1
Learning more about both the geography and the personal factors associated with opioid overdoses could help guide intervention and treatment, according to study co-author Diego Cuadros, PhD, an assistant professor at the University of Cincinnati.
“Most of the research on the opioid epidemic focuses on how to develop drugs that aren’t produced with opiates in the first place, how to produce drugs to control the overdose, or understanding why particular individuals are getting addicted,” Cuadros tells Verywell. “I wanted to have a different look at the problem.”
“We found that, although we talk about the opioid overdose epidemic in the entire country, people think this is everywhere and everybody’s at the same risk,” Cuadros adds. “It definitely is not, it is in very particular areas.”
What Areas Are Struggling With Opioids the Most?
The researchers used data collected by the Centers for Disease Control and Prevention (CDC) on fatal opioid overdoses in the United States from 2005 to 2017. They identified more than 460,000 opioid-related deaths within that time period.
“We confirmed that, basically, we don’t have the same distribution of this problem everywhere. It’s actually some particular areas, some particular hot spots, which is where the burden of the problem is very high,” Cuadros says. “These hot spots are located mainly close to the main cities, like for example, in Cincinnati, in Columbus, and also in Dayton, Ohio. So this again is very important because the key message from this study is that we need to focus the resources in those particular areas.”
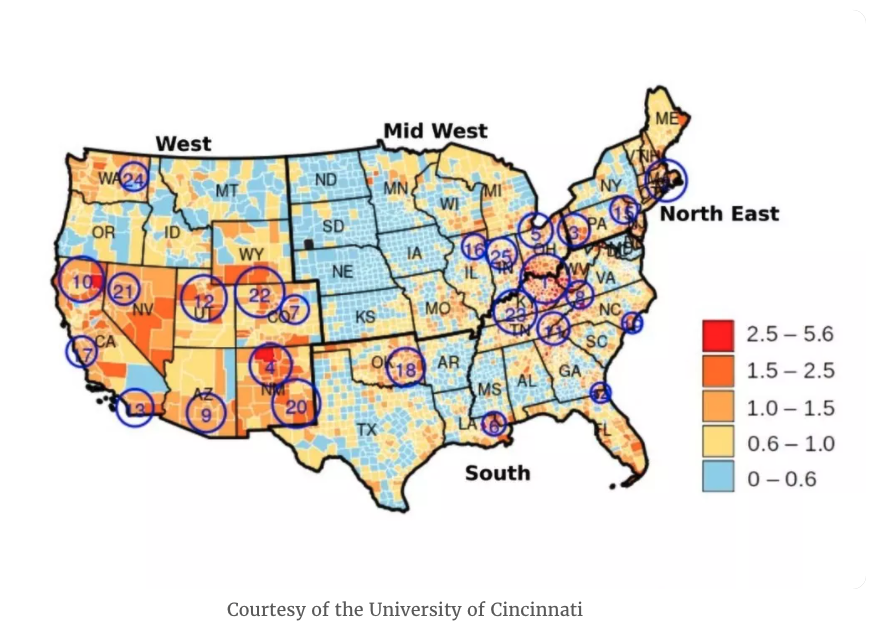
The researchers found that the states with the highest density of opioid addiction-related deaths were:
- Ohio
- Pennsylvania
- Kentucky
- West Virginia
- Indiana
- Tennessee
Who Was Most At Risk for Substance Abuse?
Beyond environment, researchers also found a few other factors that made an individual more at risk.
The researchers found that White males ages 25 to 29 were most at risk of fatal opioid overdose, followed by those aged 30 to 34. According to Cuadros, there’s still work to be done on understanding why this group specifically is the hardest hit.
However, another segment of the population is starting to see a rise in opioid-related deaths as well. Researchers saw an increased risk for Black males ages 30 to 34. “What we predict is that, very quickly, this group is going to become the main group affected by the opioid epidemic in the coming years,” Cuadros says.
The study also found a correlation between fatal overdoses and mental and physical distress. Using surveys about patients’ mental health, the researchers concluded that mental distress increases the relative risk of dying from a drug overdose by as much as 39%.
Cuadros explains that, although this correlation may seem like common sense, there hadn’t been enough data to show a solid link before. This might, arguably, be one of the most important takeaways from these findings because it once again shines a light on the hidden importance of mental health, according to Cuadros. And the COVID-19 pandemic has only exacerbated mental distress.
“The artificial separation of substance use disorder (SUD) from mental illness and medical conditions has led to a siloed healthcare delivery system,” Varun Choudhary, MD, MA, chief medical officer for behavioral health at Magellan Healthcare, tells Verywell. “It is now more important than ever to approach treatment in a comprehensive, integrated, and holistic manner to address all diseases and prevention efforts before they lead to additional unintended and dire outcomes.”
What This Means For You
If you or someone you know is struggling with substance abuse, call SAMHSA’s National Helpline, 1-800-662-HELP (4357). It’s confidential, free, and runs 24-hour-a-day, 365-day-a-year. It’s available in English and Spanish. If you call this helpline, they can give you referrals to local treatment centers, support groups, and other organizations.
Improving the Opioid Crisis Won’t Be Easy
Researchers say they now need to focus on why these specific locations are hardest hit, and why these specific subgroups of the population are most affected. “The drug addiction epidemic is more complex than, say, a virus epidemic, because you have many different agents, different drivers changing over time,” Cuadros says.
They’re hopeful these findings can help policymakers think outside the box when it comes to tailored interventions.
However, “the problem is not easy to solve,” Jagdish Khubchandani, PhD, professor of public health at New Mexico State University, tells Verywell.
Khubchandani isn’t hopeful for better results just yet. He says that, with the pandemic, opioid use may worsen unless serious and accelerated efforts are made to curb it. He suspects that data from 2018 onwards will continue to show results on this trajectory of growth.
“While the White House declared opioid use as a public health emergency, there are fewer boots on the ground and fewer initiatives than desirable,” Khubchandani says. “Multipronged and interdisciplinary approaches are needed to reduce this problem.”
Some key interventions, according to Khubchandani, should include:
- Improving access to healthcare
- Recruiting and retaining mental health professionals for rural America
- Quality rehabilitation
- Improving the social determinants in these areas
“Hopefully, studies like the above can help find new ways to tackle the issue,” he says.
- Hernández A, Lan M, MacKinnon NJ, Branscum AJ, Cuadros DF. “Know your epidemic, know your response”: Epidemiological assessment of the substance use disorder crisis in the United States. PLoS One. 2021;16(5):e0251502. doi:10.1371/journal.pone.0251502
